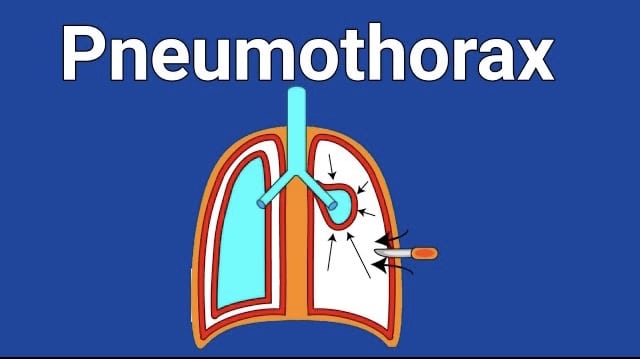
Pneumothorax is a medical condition characterize by the presence of air or gas in the pleural cavity, the space between the lungs and the chest wall.
This accumulation of air in the pleural cavity can cause the lung to collapse partially or completely leading to difficulties in breathing and other symptoms.
Types of Pneumothorax
There are two main types :
Spontaneous Pneumothorax:
This type occurs without any traumatic injury to the chest and is further classified into two subtypes:
- Primary Spontaneous Pneumothorax:
This occurs in individuals without any underlying lung disease or apparent cause. It often happens in tall, thin individuals.
- Secondary Spontaneous Pneumothorax:
This occurs in individuals with underlying lung diseases, such as chronic obstructive pulmonary disease (COPD), asthma, tuberculosis, cystic fibrosis, or lung cancer.
Traumatic Pneumothorax:
This type is caused by a traumatic event or injury, such as a car accident, a penetrating chest wound, or a broken rib that punctures the lung.
Pneumothorax Symptoms
The symptoms of pneumothorax can vary depending on the size of the air leak and the extent of lung collapse.
Common symptoms include sudden sharp or stabbing chest pain, shortness of breath, rapid breathing, rapid heart rate, cyanosis (bluish discoloration of the skin), and decreased breath sounds on the affected side.
Diagnosis
The diagnosis of typically involves a combination of medical history review, physical examination, and imaging tests.
Here is a step-by-step overview of the diagnostic process for pneumothorax:
Medical History:
Your doctor will begin by asking about your symptoms, medical history, and any recent traumatic events or lung conditions you may have.
This information helps in understanding the potential causes and risk factors associated with pneumothorax.
Physical Examination:
During the physical examination, your doctor will listen to your lungs using a stethoscope to assess breath sounds.
They will also examine your chest for signs such as asymmetrical chest movements during breathing.
Decreased breath sounds on the affected side, and abnormal resonance when tapping on the chest wall.
Imaging Tests:
- Chest X-ray:
This is often the first imaging test performed to confirm the presence of pneumothorax.
It can show air in the pleural cavity and reveal the extent of lung collapse.
A characteristic finding on a chest X-ray is the presence of a dark area with absent lung markings on the affected side.
- Computed Tomography (CT) Scan:
In some cases, a CT scan may be order, especially when a small pneumothorax is suspect, or there is a need for more detail imaging.
A CT scan provides cross-sectional images of the chest, allowing for a more precise evaluation of the pneumothorax and any underlying lung pathology.
- Additional Tests:
Depending on the specific situation, additional tests will be perform to evaluate the underlying cause or associated complications of pneumothorax.
These tests may include blood tests, pulmonary function tests, or bronchoscopy (a procedure to examine the airways).
It’s worth noting that in certain emergency situations where a large pneumothorax causes severe symptoms or unstable vital signs
The diagnosis may be made based on clinical signs and immediate management initiated without waiting for imaging confirmation.
If you suspect you have a pneumothorax or are experiencing symptoms such as sudden chest pain and difficulty breathing, it is crucial to seek medical attention promptly.
A healthcare professional will be able to evaluate your condition, perform the necessary tests, and provide appropriate treatment.
Medical Treatment
The treatment for pneumothorax depends on the severity of the condition, the size of the pneumothorax, the presence of symptoms, and the underlying cause.
Here are the common approaches to treating pneumothorax:
Observation:
Small, uncomplicated pneumothoraxes may not require immediate intervention and can be manage through observation.
In these cases, the doctor will closely monitor your condition with regular chest X-rays to ensure the pneumothorax resolves on its own.
You may be advise to avoid activities that can increase air pressure in the chest, such as flying or scuba diving, until the pneumothorax is resolve.
Aspiration:
If the pneumothorax is large or causing significant symptoms, your doctor may perform a procedure called aspiration or needle aspiration.
Under local anesthesia, a needle or catheter will insert into the chest cavity to remove the excess air.
This helps relieve pressure and allows the lung to re-expand.
Aspiration is typically follow by a chest X-ray to confirm lung re-expansion.
Chest Tube Insertion:
For larger or persistent pneumothoraxes, a chest tube may be inserted.
This procedure, known as tube thoracostomy, involves placing a flexible tube through a small incision in the chest wall into the pleural cavity.
The tube will connect to a suction device or drainage system to remove the air and assist the lung in re-expanding.
Chest tube insertion is usually will be perform under local anesthesia or with sedation.
Pleurodesis:
Pleurodesis is a procedure which will perform to prevent recurrent pneumothorax.
It involves creating adhesions between the lung and the chest wall, sealing the pleural space and preventing air from accumulating.
This can be done by introducing a medication, such as talc, through a chest tube, or by surgical methods.
Surgery:
In some cases, surgery may be necessary to treat pneumothorax.
Surgical interventions are typically consider when other treatments have failed, or if there are underlying lung conditions that require surgical management.
The surgical procedures include video-assisted thoracoscopic surgery (VATS) or open thoracotomy.
which aim to repair any underlying lung blebs or bullae and prevent recurrent pneumothorax.
Pneumothorax physiotherapy treatment
Physiotherapy plays a supportive role in the management of pneumothorax, particularly during the recovery phase.
While physiotherapy cannot directly treat or resolve a pneumothorax, it can help improve respiratory function, promote lung re-expansion.
And aid in the overall recovery process. Here are some physiotherapy treatments commonly used for pneumothorax:
Breathing Exercises:
Deep breathing exercises can help improve lung function and promote lung re-expansion.
Your physiotherapist may teach you techniques such as diaphragmatic breathing, pursed-lip breathing, and incentive spirometry.
These exercises aim to increase lung capacity, improve oxygenation, and assist in the removal of secretions.
Chest Physiotherapy:
Chest physiotherapy techniques can help mobilize secretions and promote effective coughing to clear the airways.
This may include percussion (gentle tapping) and postural drainage, where specific positions are used to drain mucus from different areas of the lungs.
These techniques are typically performed under the guidance of a physiotherapist.
Exercise and Physical Activity:
Gradual re-introduction of physical activity can be beneficial for overall respiratory fitness and lung function.
Your physiotherapist may provide guidance on appropriate exercises and activities to gradually rebuild strength and endurance.
while considering your individual condition and any underlying lung issues.
Education and Lifestyle Modification:
A physiotherapist can provide education on posture, body mechanics, and lifestyle modifications to optimize breathing and reduce the risk of recurrent pneumothorax.
This may include advice on maintaining good posture, avoiding activities that increase the risk of pneumothorax (e.g., smoking, scuba diving) and recognizing warning signs that require medical attention.
Support and Rehabilitation:
Physiotherapy can provide emotional support and motivation during the recovery phase.
Your physiotherapist can offer guidance on coping strategies, stress management, and lifestyle adjustments to help you regain your physical and emotional well-being.
It is important to note that physiotherapy interventions for pneumothorax should be tailored to the individual’s specific condition
And guided by a healthcare professional. Always consult with your healthcare team, including a physiotherapist, to develop an appropriate treatment plan based on your needs and overall recovery goals.
Read Our intresting article on Pleural Effusion , Kindly click here